Abstract

Background: The prognosis of central nervous system (CNS) involvement in adult patients with acute lymphoblastic leukemia (ALL) has been historically associated with a dismal outcome. Whereas the prognosis of adult patients with ALL has greatly improved since the advent of pediatrics-inspired regimens, the prognostic impact of CNS involvement has not been formerly reevaluated. We report herein the impact of CNS involvement in patients included in the pediatric-inspired prospective GRAALL-2005 study.
Methods: All patients received a 5-drug induction therapy with native E. Coli-ASP intravenous injections. Patients in complete remission (CR) received two consolidation courses with alternating cycles including high dose cytarabine (2g/m2/12h on days 1 and 2), high dose methotrexate (3 g/m2 on day 1), and cyclophosphamide. All patients in persistent CR and with no indication for allogeneic stem cell transplantation (SCT) received late intensification, followed by one last consolidation course. Patients with initial CNS involvement, clinically and/or cytologically (cerebrospinal fluid), were recommended to receive an increased number of triple intrathecal therapy, CNS irradiation, and were eligible for allogeneic SCT in first CR. They received less Asp injections during induction therapy to avoid CNS adverse events. CNS irradiation included two lateral fields encompassing the skull, facial, the base of the skull, and the first two cervical vertebrae at a dose of 24 grays for those not receiving allogeneic SCT and 15 grays for those receiving allogeneic SCT.
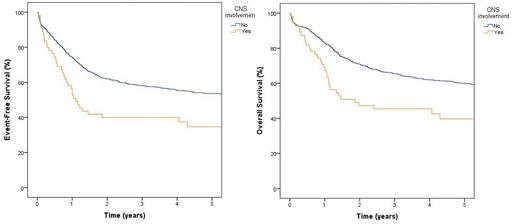
Results: Between 2006 and 2014, 784 adult patients with newly diagnosed Philadelphia-negative ALL were included with 55 (7%) having initial CNS involvement. These patients were more likely to be of T-phenotype (51 versus 32%, p=.004) and had more white blood cells at diagnosis (median 23 G/l versus 11 G/l, p=.02). Most patients (36 pts, 66%) were classified as CNS-3 (> 5 white blood cells/µl and a positive cytospin and/or clinical signs) whereas 5 patients (9%) were CNS-2 (< 5 white blood cells/µl and a positive cytospin), and 14 (25%) have data pending. Among patients with details regarding CNS involvement, 25/41 (61%) had clinical signs including trigeminal anesthesia (9 pts, 36%), facial paralysis (4 pts, 16%), extremities paresthesia (4 pts, 16%), visual signs (2 pts, 8%), meningeal syndrome (2 pts, 8%), and motor deficit (2 pts, 8%), and 4/18 (22%) had radiological signs. Induction death, CR1 rate, and negative minimal residual disease after induction were similar whether patients had CNS involvement or not (6 vs 6%, 89 vs 89%, 73 vs 62%, 26 vs 22%, respectively). Patients with CNS involvement had a worse outcome than those without with a median event-free survival (EFS) of 391 days (versus not reached for patients without CNS involvement, HR: 1.7, 95% CI: 1.2 - 2.5, p=.002) and a median overall survival (OS) of 608 days (versus not reached for patients without CNS involvement, HR: 1.8, 95% CI: 1.3 - 2.6, p=.001) (figure). Similar results were observed when patients who received allogeneic SCT in CR1 were censored at the time of graft. As recommended, patients with CNS involvement were more likely to receive allogeneic SCT than those without (53 versus 34%, p=.01), with a median time of 169 days. A 150-day landmark analysis, excluding 12 patients with an EFS event before 150 days, was performed to study the impact of allogeneic SCT on the outcome of patients with CNS involvement. Allogeneic SCT had no impact on either EFS (HR: .5, 95% CI: .2 - 1.2, p=.15) or OS (HR: .8, 95% CI: .3 - 1.8, p=.53).
Conclusion: Despite improved outcome in young adult ALL patients with pediatrics-inspired protocols, CNS involvement remains a poor-risk feature. The historical use of allogeneic SCT does not improve outcome. Specific regimens should be developed for adult ALL patients with CNS involvement.
Huguet: Amgen: Other: Advisor; BMS: Other: Advisor; Celgene: Other: Advisor; Jazz Pharmaceuticals: Other: Advisor; Novartis: Other: Advisor; Pfizer: Other: Advisor. Barbieux: ASTRA-ZENECCA: Consultancy. Vey: Amgen: Honoraria; BMS: Honoraria; BIOKINESIS: Consultancy, Research Funding; NOVARTIS: Consultancy, Honoraria, Research Funding; SERVIER: Consultancy; JAZZ PHARMACEUTICALS: Honoraria; JANSSEN: Consultancy. Dombret: Amgen: Honoraria, Research Funding; Incyte: Honoraria, Research Funding; Jazz Pharmaceuticals: Honoraria, Research Funding; Novartis: Research Funding; Pfizer: Honoraria, Research Funding; Servier: Research Funding; Abbvie: Honoraria; BMS-Celgene: Honoraria; Daiichi Sankyo: Honoraria. Boissel: Bristol-Myers Squibb: Honoraria, Research Funding; Servier: Consultancy, Honoraria; Incyte: Honoraria; Amgen: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; JAZZ Pharma: Honoraria, Research Funding; CELGENE: Honoraria; SANOFI: Honoraria; PFIZER: Consultancy, Honoraria. Mathilde: ABBVIE: Consultancy; SERVIER: Consultancy.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal